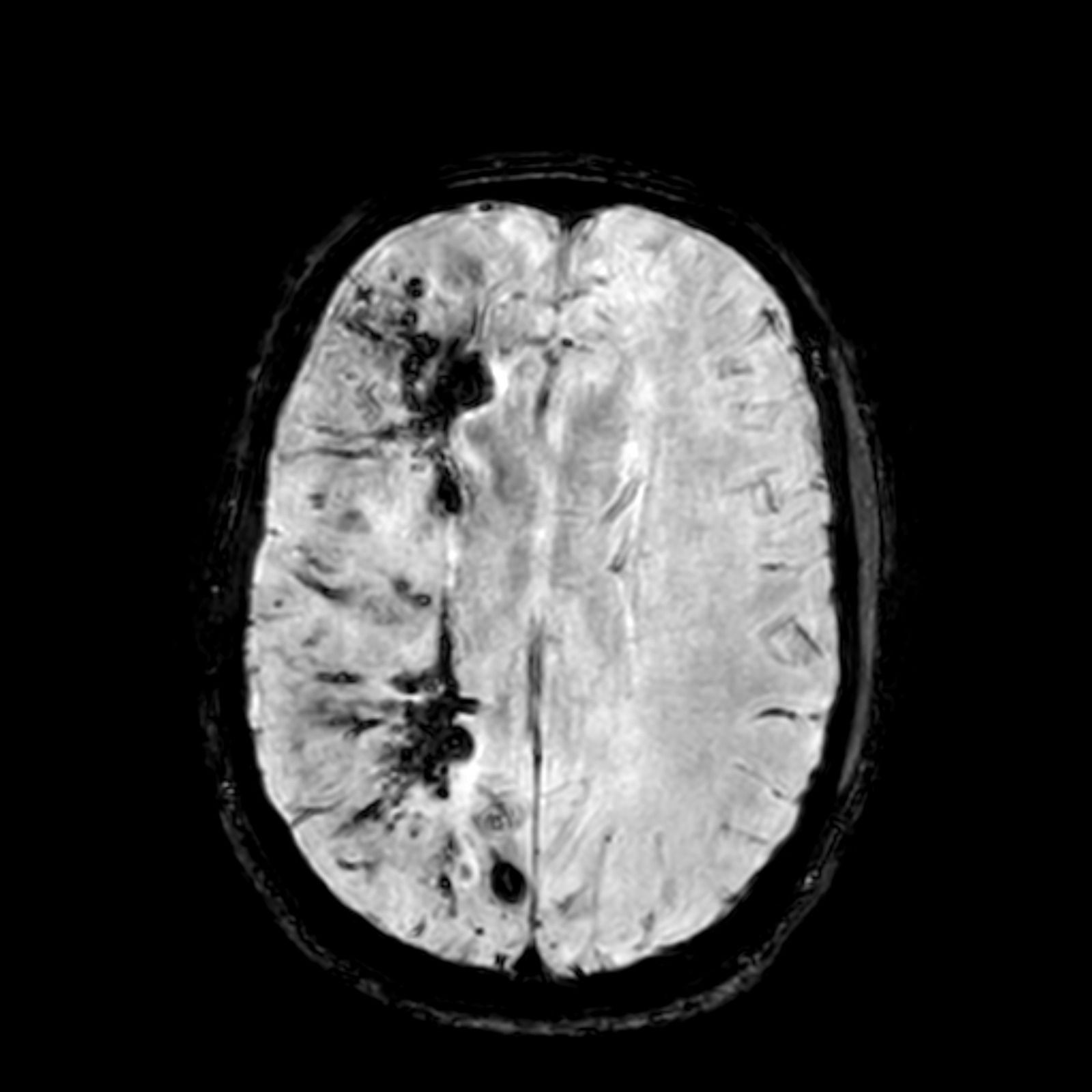
Overview of cerebral cavernous malformations: comparison of treatment approaches
Citation: Bubenikova A, Skalicky P, Benes V Jr, Benes V Sr, Bradac O. Overview of cerebral cavernous malformations: comparison of treatment approaches. J Neurol Neurosurg Psychiatry. 2022 May;93(5):475-480. doi: 10.1136/jnnp-2021-328658. Epub 2022 Mar 10. PMID: 35273070.
This work presents the issue of treatment of cerebral cavernous malformations (CCMs) in terms of intervention and observation. A meta-analysis and systematic review were performed involving 98 primary publications with a total of 100 cohort studies yielding 8994 patients who underwent surgery, radiosurgery, or conservative treatment with the disease during 1990−2020. All this work was subject to precise methodological rules according to the official PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) documentation. The risk of bias in the analysed studies was assessed using Newcastle-Ottawa Scale (NOS). Exclusively studies with a high or medium risk of bias (≥ 6 * according to NOS) were included in the final statistical analysis. The main aim of the statistical processing was to (1) calculate overall haemorrhage rate, case fatality and long-term in each predefined treatment modality, (2) specify the treatment efficacy and mortality/morbidity rate by calculating the cumulative incidence with corresponding 95% confidence intervals (CIs) for each outcome using the random effects model, and (3) investigate further associations among patients’ demographics and posttreatment haemorrhage rate by calculating adjusted rate ratios with 95% CIs according to Poisson’s distribution models. Finally, sensitivity analyses of overall case fatality and haemorrhage rates were conducted in high-quality cohorts, i.e., those with prospective design or in which the outcome of interest was not present at the start of the study. The heterogeneity test was performed using Cochran’s Q and I2 statistics. All computations were performed with MetaXL and STATISTICA software.
The efficacy of ensuring the prevention of haemorrhage was 97% in surgical, 86% in radiosurgical and 77% in the conservative treatment. The lowest mortality (1%) was after radiosurgery, and the highest persistent morbidity (22%) was in natural history series. Deep-seated and brainstem CCMs were associated with higher bleeding rates. Lobar localisation was a protective factor in all analyses. Patients with history of previous haemorrhage were exposed to higher risk of rebleeding. Male gender was a protective factor associated with lower risk of post-treatment haemorrhage.