Structural volumetry in NPH diagnostics and treatment – future or dead end?
Citation: Vlasák A, Skalický P, Mládek A, Vrána J, Beneš V, Bradáč O. Structural volumetry in NPH diagnostics and treatment-future or dead end? Neurosurg Rev. 2021 Feb;44(1):503-514. doi: 10.1007/s10143-020-01245-y. Epub 2020 Jan 24. PMID: 31980974.
This study was perform with a goal to assess automated volumetric analysis as a potential presurgical diagnostic tool or as a method to potentially shed light on normal pressure hydrocephalus (NPH) pathophysiology. MRI imaging according to our protocol was performed in 29 NPH patients, 45 non-NPH (but suspected) patients and 15 healthy controls. Twenty patients underwent a second MRI 3 months after ventriculoperitoneal (VP) shunt surgery.
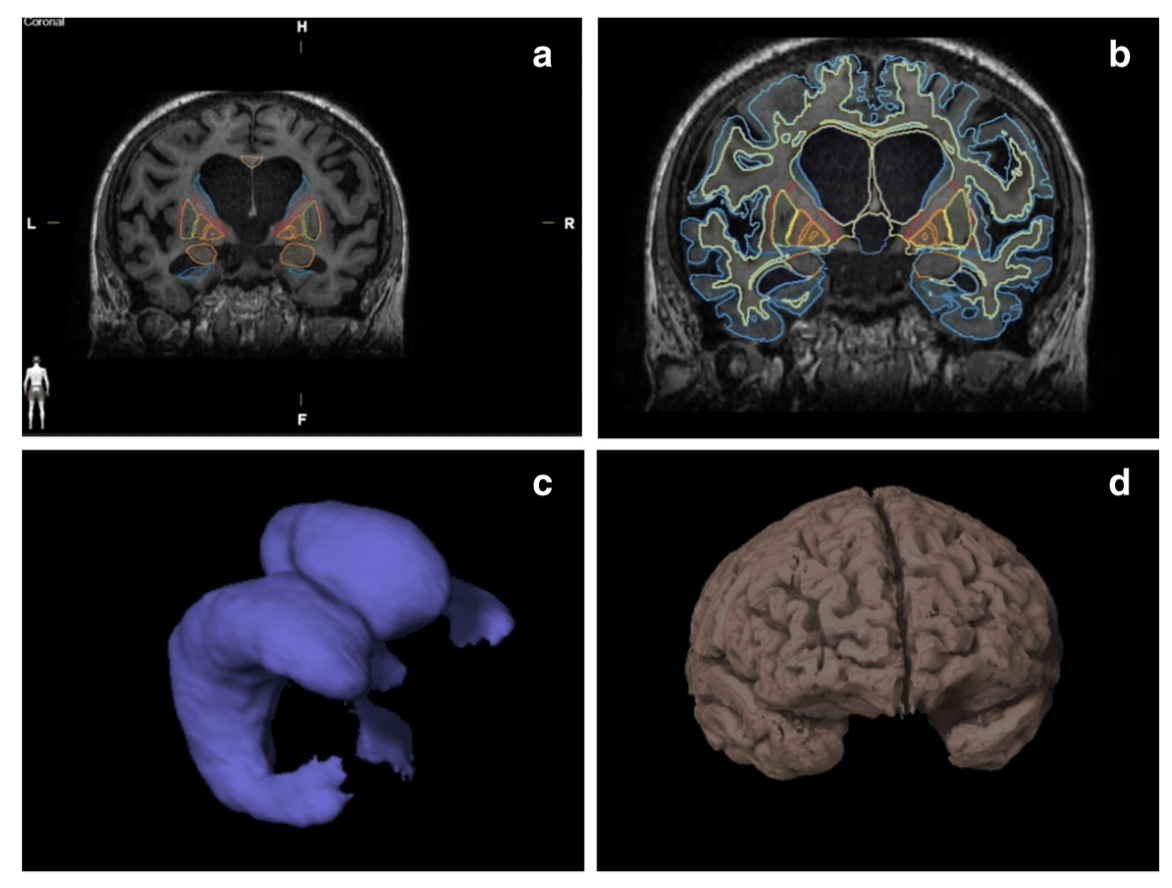
All structures relevant to NPH diagnosis were automatically segmented using Anatomical Mapping 1.1 as a part of Brainlab Elements software. We have successfully measured volumes of both white and grey matter, internal and external capsule, corpus callosum, hippocampus, amygdala, caudate nucleus, putamen, internal and external globus pallidus, thalamus, periaqueductal grey and three ventrucles. The fourth ventricle was manually removed from the ventricular system measurement in the level of the cerebral aqueduct because its volume is not related to NPH diagnosis. The results were subsequently tested using ANOVA analysis. Significant differences in the volumes of the corpus callosum, left hippocampus, internal globus pallidus, grey and white matter and ventricular volumes were observed between NPH group and healthy controls. However, the differences between NPH and non-NPH groups were non-significant. Three months after, VP shunt insertion decreased ventricular volume was the only clearly significant result (p value 0.0001).